ICE-T Inpatient Cost Evaluation Tool
Understanding Bundled Payments
Bundled payments are an alternative to traditional fee-for-service (FFS) payments for patient health care. Instead of basing reimbursements on the cost of each specific service associated with an episode of care, which may have high variance for both payers and providers, the payer is charged a flat fee for an inpatient diagnosis-related group (DRG) episode, regardless of the cost, which takes into account the frequency and variance of the episode cost. The goal is to reduce overall health care costs while still covering the costs incurred by providers, such as physicians and hospitals.
Bundled payment prices are usually set around the mean cost of the DRG for an episode, although providers can negotiate different prices with their payers. The Centers for Medicare and Medicaid Services (CMS) typically rely upon a bundled payment benchmark price of the expected value, or mean cost, of the DRG episode minus 5 percent to incentivize reductions in health care costs. However, with the exception of DRGs 469 & 470 (hip and knee replacement surgeries), providers currently submit individual proposals to CMS detailing which DRGs they would like to bundle, a proposed bundle price, and any provisions for managing risk. This provides some flexibility to providers to negotiate prices that incorporate idiosyncratic provider risks, such as those associated with their practice panel size or underlying patient panel characteristics.
Many practices are concerned about the risks associated with bundled payments because they are reimbursed the same amount for all episodes regardless of the medical severity or intensity of service utilization in the episode – especially if the bundled price carries a 5 percent discount to the true mean episode cost.
For example, the figure below shows a typical distribution of DRG episode costs that a provider may face. For most DRGs, there are a large share of patients with relatively moderate costs before a long right tail of episodes that occur infrequently but have very high costs. While the most likely cost of an episode occurs at the peak of the distribution, the actuarially fair bundled price would be the expected value, or mean cost, indicated to the right of peak.
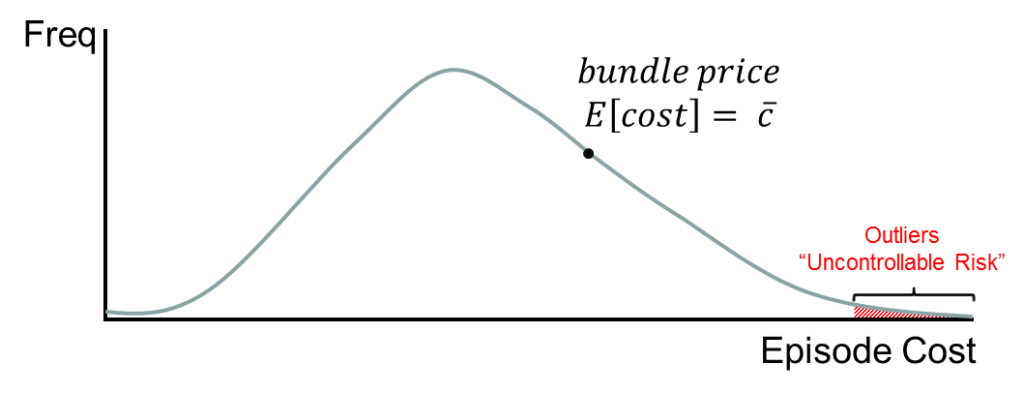
At this reimbursement point, providers facing this distribution of episodes would receive higher reimbursements than needed to cover the cost of care for all episodes to the left of the bundled price, which would be exactly high enough to cover the additional costs not covered by the bundle price reimbursement for all of the episodes to the right of the bundled price. Thus, a correctly calculated bundle payment manages all of the risk to providers.
CMS typically includes a 5 percent discount to the bundled price to incentivize practices to reduce waste by curbing low value procedures. That said, payers and providers both agree there are expensive outlier episodes that occur because of comorbidities or other complexities that are beyond a provider’s control. These are indicated as “uncontrollable risk” in the figure. An actuarially fair bundle price covers the costs of these outlier episodes – but only if a practice has a large enough patient panel to accurately estimate the actuarially fair price.
The Neiman Institute is reviewing methods to protect practices – especially small practices – from the financial risk associated with bundled payments.
It is therefore important to compare your practice population and costs to the national average!
Smaller practices, for example, may face higher variance in their patient populations and may therefore have a mean cost for patient care significantly higher than the national average. If your practice costs for a given DRG are less than the national benchmark set by CMS, there is the potential to benefit from bundle payment models. However, if your practice costs are significantly higher than the national benchmark, it may be better not to bundle, or to engage in risk mitigation techniques if you do.
In November 2015, CMS ruled that it will require hospitals in 67 geographic areas to participate in a test of bundled payments for hip and knee replacements (DRG 469 & DRG 470), implemented in April 2016. The reimbursements that CMS will make for these DRGs are set to regional benchmarks to better account for local variation in patient health. More DRGs are expected to be bundled in the next few years. In the meantime, providers can propose bundling other DRGs as part of the Bundled Payments for Care Improvement Initiative (BPCI).
Risk Mitigation in Bundled Payments