ICE-T Inpatient Cost Evaluation Tool
Frameworks for Radiology Practice Participation
Given the many different independent providers involved in most inpatient episodes, there are multiple ways inpatient bundled payment models can be organized. All bundled payment models have a single designated provider organization that is responsible for the quality and cost of the entire episode.
Hospitals are frequently the responsible provider for inpatient episodes with some episodes, such as the Comprehensive Care for Joint Replacement (CJR) model, requiring hospitals to serve in this role. For simplicity, we assume here that hospitals will serve as the responsible provider. However, these organizational concepts can easily be modified by substituting different providers where appropriate.
The best framework for radiology practice participation often depends upon whether the inpatient episode is being reimbursed through either a retrospective or prospective bundled payment.
Retrospective Bundled Payment Frameworks
Under retrospective bundled payments, all providers file fee-for-service (FFS) claims as normal. At the end of an annual performance period, the aggregate costs for the episode from all providers are compared to the benchmark cost for that episode. The responsible provider, such as a hospital, then either receives a portion of any savings that accrue relative to the benchmark cost or must reimburse CMS for costs exceeding the benchmark cost. Although this model incentivizes responsible providers to control costs, what role do radiology practices play in this bundle?
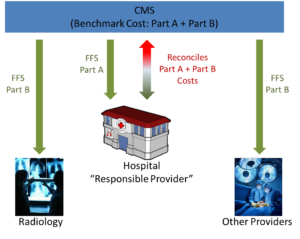
Scenario 1: Responsible Provider is “In” the Bundle
With this framework, radiology practices do nothing. Radiology practices and other non-hospital providers are simply reimbursed under FFS and the hospital is accountable for whether the total cost meets or exceeds the CMS’s benchmark – even if there are significant Part B costs driven by non-hospital providers.
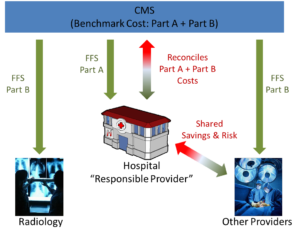
Scenario 2: Hospitals and Non-Radiology Primary Care Providers are “In” the Bundle
In this framework, hospitals and non-radiology providers agree to share in both the savings and risk of the annual reconciliation. Hospitals are still designated the responsible provider for the episode and perform the reconciliation with CMS. After this reconciliation occurs, hospitals then pass along a pre-negotiated share of savings to the primary care providers, or collect a share of the reimbursement CMS requires from these providers. This incentivizes primary care providers to better manage total episode costs but it also requires detailed data to determine how to spread the risk and any potential savings between hospitals and primary care providers. Radiology practices continue to receive FFS payments with no risk. However, radiology practices may experience a decrease in imaging orders from primary care providers directly participating in the bundle as these providers seek to reduce episode costs, and potentially compromise the patient’s quality of care.
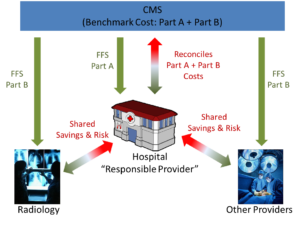
Scenario 3: All Providers are “In” the Bundle
Hospitals can also employ models where all of the primary care providers are in the bundle. All providers continue to receive FFS payments and the hospital must reconcile the total episode cost with the CMS benchmark. However, all providers now agree to share in the risk and rewards with the hospital. This model allows radiology practices to actively participate in the bundle to reduce unnecessary imaging while ensuring the quality of patient care. Participation in this model requires detailed data on total episode costs and its constituent radiology costs, non-radiology provider cost, and hospital costs to determine the appropriate share of risk and savings for each provider in the episode.
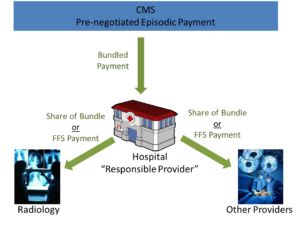
Prospective Bundled Payment Frameworks
Under prospective bundled payments, the responsible provider (the hospital) receives a single pre-negotiated payment from the payer for all services associated with a patient episode. The responsible provider incurs all of the risk for the episode but also receives all of savings that may accrue.
The organizational frameworks for prospective bundles are very similar to those under retrospective bundles. However, all of the non-responsible providers file claims directly to the hospital and are reimbursed directly by the hospital out of the bundled payment that the hospital receives.
Non-hospital providers may either receive FFS payments, a pre-negotiated fixed payment for the episode, or a pre-negotiated percentage of the bundled reimbursement.
Prospective bundled payments offer a few different opportunities and potential problems for radiology practices. For example, if other primary care providers are receiving a share of the bundle while radiology practices are submitting FFS claims to the hospital, other primary care providers may be incentivized to save costs by drastically reducing imaging orders and potentiality compromising patient care.
On the other hand, if radiologists agree to a single pre-negotiated payment or share for all imaging services in an episode, other primary care providers may order more images than appropriate, because they receive all of the imaging they want for the same fixed payment. While radiology practices will have incentives to work with other providers to identify and recommend against inappropriate imaging, radiologists’ ability to reduce inappropriate imaging is limited by their potential exposure to malpractice suits and local tort liability.
Other Organizational Frameworks
The frameworks described above are the most common methods of organizing participation in different bundled payment models. Ultimately, providers may choose from any of these or develop other variants and hybrids of these frameworks. Whether a radiology practice decides to participate in a bundled payment model and which model makes the most sense for a radiology practice will depend upon the specific DRG; the relationships between the radiology practice, the hospital, and other providers in the episode; degree of variance in radiology services for the DRG; the average imaging cost for an episode; and the share of the total episode cost from radiology.
It is vital for radiology practices to examine their own data and compare it to benchmarks such as those found in the ICE-T application before engaging in risky bundled payment contracts.
Practice concerns about over-utilization or harmful under-utilization of imaging can be mitigated through computerized decision support (CDS) systems that embed evidence-based appropriateness criteria. Discussions with hospitals about the use of CDS systems should be an important part of any bundled payment negotiations and may mitigate the risk radiology practices face in these payment models.