January 20, 2025
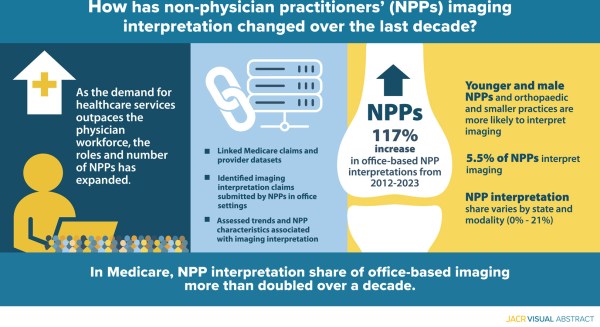
Diagnostic imaging interpretations by nonphysician practitioners (NPPs) are increasing. With hospital-based imaging overwhelmingly interpreted by radiologists, the researchers studied office-based interpretations by NPPs by their physician employer specialty. View Infographic
As indications for acute ischemic stroke treatment expand, it is unclear whether disparities in treatment utilization and outcome still exist. The main objective of this study was to investigate disparities in acute ischemic stroke treatment and determine impact on outcome. Full Article
Jeffrey M. Katz, MD , Jason J. Wang, PhD, Maria X. Sanmartin, PhD, Jason J. Naidich, MD, MBA, Elizabeth Rula, PhD, Pina C. Sanelli, MD, MPH. 2024. "Ten-year trends, disparities, and clinical impact of stroke thrombectomy and thrombolysis: a single center experience 2012-2021," Journal of Stroke and Cerebrovascular Diseases
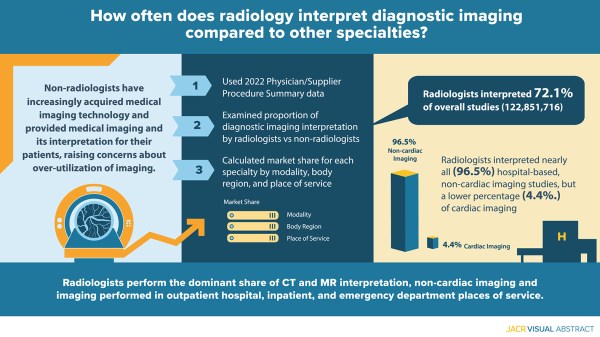
The aim of this study was to examine radiology’s and other specialties’ market shares for diagnostic imaging interpretation for Medicare fee-for-service claims by modality, body region, and place of service. Full Article
Eric W. Christensen, PhD, Elizabeth Y. Rula, PhD, Jeffrey H. Newhouse, MD. 2024. "Share of Diagnostic Imaging Interpretation: Radiology and Other Specialties," Journal of the American College of Radiology (JACR)
June 28, 2024
The aim of this study was to examine radiology’s and other specialties’ market shares for diagnostic imaging interpretation for Medicare fee-for-service claims by modality, body region, and place of service. Authors: Eric W. Christensen, PhD, Elizabeth Y. Rula, PhD, Jeffrey H. Newhouse, MD Read the JACR study for full details.
A range of economic and health policy incentives are leading to ongoing consolidation among payers, hospitals, and physician practices. The objective of this study is to evaluate consolidation among radiologists' affiliated practices through 2023, analyze the impact of consolidation on such practices' specialty mix and size, and assess radiologists' new affiliations after prior practices cease. Full Article
Eric W. Christensen, PhD, YoonKyung Chung, PhD, Elizabeth Y. Rula, PhD, Jay R. Parikh, MD. 2024. "Changes in the Radiology Practice Landscape and Indicators of Practice Consolidation From 2014 to 2023," American Journal of Roentgenology
Volume increases, inflation, statutory freezes in physician payments, and the budget neutrality requirement for the Medicare Physician Fee Schedule have resulted in persistent inflation-adjusted conversion factor decreases. This study aimed to determine if relative value unit (RVU) volume increases on a per beneficiary basis has counteracted conversion factor decreases and inflation to maintain Medicare reimbursement per beneficiary, overall and across specialties. Full Article
Eric W. Christensen, PhD, Gregory N. Nicola, MD, Elizabeth Y. Rula, PhD, Lauren P. Nicola, MD, Joshua A. Hirsch, MD. 2024. "Medicare Volume Growth and Shift in Payments From Physicians to Non-Physician Practitioners Under Statutory Budget Neutrality," INQUIRY: The Journal of Health Care Organization, Provision, and Financing
Medical imaging, identified as a potential driver of unsustainable US health care spending growth, was subject to policies to reduce prices and use in low-value settings. Meanwhile, the Affordable Care Act increased access to preventive services—many involving imaging—for employer-sponsored insurance (ESI) beneficiaries. The researchers used a large insurance claims database to examine imaging spending trends in the ESI population between 2010 and 2021—a period of considerable policy and benefits changes. Full Article
Michal Horný, Daniel Chang, Eric W Christensen, Elizabeth Y Rula, Richard Duszak, Jr. 2024. "Decomposition of Medical Imaging Spending Growth Between 2010 and 2021 in the U.S. Employer-Insured Population (Michal Horny)," Health Affairs Scholar
To propose a research method for identifying “practicing interventional radiologists” using 2 national claims data sets. Full Article
Mikki D. Waid, PhD, Elizabeth Y. Rula, PhD, Matthew Hawkins, MD, Laura Findeiss, MD, Raymond Liu, MD. 2024. "A Claims-Based Method for Identification and Characterization of Practicing Interventional Radiologists," Journal of Vascular and Interventional Radiology (JVIR)
Prudent imaging use is essential for cost reduction and efficient patient triage. Recent efforts have focused on head and neck CTA in patients with emergent concerns for non-focal neurological complaints, but have failed to demonstrate whether increases in utilization have resulted in better care. The objective of this study was to examine trends in head and neck CTA ordering and determine whether a correlation exists between imaging utilization and positivity rates. Full Article
Grant H. Rigney, Alexander H. King, Janice Chung, Soham Ghoshal, Aditya Jain, Zhuo Shi, Shahaan Razak, Joshua A. Hirsch, Michael H. Lev, Karen Buch & Marc D. Succi. 2024. "Trends in Non-Focal Neurological Chief Complaints and CT Angiography Utilization among Adults in the Emergency Department," Internal and Emergency Medicine
March 12, 2024
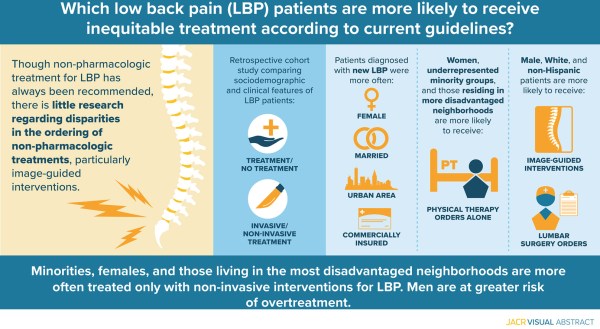
This study assessed individual- and neighborhood-level sociodemographic factors associating with providers’ ordering of nonpharmacologic treatments for patients with low back pain (LBP), specifically physical therapy, image-guided interventions, and lumbar surgery. Authors: Miriam E. Peckham, MD, Lubdha M. Shah, MD, MS, Huong D. Meeks, PhD, MStat, MPH, Alison Fraser, MSPH, Carlos Galvao, BS, Ghazaleh Safazadeh, MPH, View Infographic