November 7, 2014
Beyond Fee-For-Service: Emerging Payment Models in Radiology
This report highlights two emerging models being developed by the Neiman Institute designed to align provision and payment of specialty care with efforts to ensure a sustainable, high quality health care system.
Introduction
Many initiatives are underway to redesign health care delivery and payment systems to curb rising costs while maintaining, and ideally improving, the overall quality of care. Whether in the form of Accountable Care Organizations, Patient-Centered Medical Homes, or various other models for payment reductions coupled with shared-savings incentives, the common feature of these systems is an increased shift of risk—for both cost and quality—to providers.
Although most early efforts have focused on integrated care delivery models, with primary care providers at the center serving as gate-keepers to manage service utilization, powerful opportunities exist for physician specialists as well. This Neiman Report highlights two of several emerging models being developed by the Harvey L. Neiman Health Policy Institute designed to align provision and payment of specialty care with efforts to ensure a sustainable, high quality health care system.
Inpatient Hospitalization Care
Inpatient hospital care has become an attractive target for redesigned payment systems. The longstanding Medicare Severity Diagnosis Related Groups (MS-DRG) system, which defines inpatient episodes for different and distinct diagnoses, offers considerable opportunities for incentivizing higher quality and lower cost specialty care. Inpatient services can be identified and defined in a fairly straightforward manner. Outpatient episodes typically feature fragmented care across a broad spectrum of providers, each with limited information on how they fit into the patient’s overall health care picture. Inpatient episodes, though imperfect, are sufficiently standardized so that data analytics can support the development of alternative delivery and payment systems.
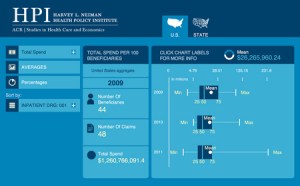
An important first step is to understand the degree to which various specialists are currently involved in inpatient care. To date, this step has received little attention. Consider the use of imaging services in MS-DRG 062 which covers specific episodes of Acute Ischemic Stroke. Our early work has focused on 5 percent Medicare Part A Limited Data Set (LDS) files for 2011 that contain all claims associated with approximately 2.6 million Medicare fee-for-service beneficiaries. An example of the insights revealed about spending associated with medical imaging is shown in Table 1.
 |
| click image to enlarge |
Of particular note is the tremendous variability in the share of imaging costs in these episodes. Moreover, the mean value (that is, the expected cost of a typical episode) is much closer to the 75th percentile than the median. This indicates that the average cost of care is heavily influenced by a relatively small number of very expensive encounters rather than the most common episodes. Drilling down to lower levels of aggregation across all 744 MS-DRGs (e.g., by state, county, or type of institution) could allow providers to directly benchmark their own services. Thus, opportunities exist to identify specific MS-DRGs where specialists may be able to either manage increased risk under bundled payment or shared-savings models. These opportunities become increasingly robust when analytics are extended to multiple service years, resulting in more statistically valid results, and to Part B claims data, as in our future research. Having such information available in mobile applications will permit providers, health systems, and payers alike to review it in a real-time interactive format. Prototype analytics tools are already being developed (Figure 1).
The real power of such inpatient episode analytics, however, is not as much in aggregate measures but rather in the ability to mine lower level claims data. For example, individual providers who are consistently beneath the typical spending distribution—but whose outcomes are similar to or better than peers—could be identified. Targeted study of their care would provide empiric outcomes information and create rich opportunities to share best-practice care delivery methods with similar specialty providers. Moreover, a similar approach could be used to identify providers whose costs and/or outcomes are consistently less favorable. Excessive, unjustifiable, or low utility care by under-performing providers could support the need for focused education using the experience of the higher performers.
Episodic Imaging Care
Defining a dedicated imaging episode of care is challenging, given that 1) imaging is integral to many varied clinical episodes, 2) imaging is often requested by multiple different treating providers during an episode of care, and 3) radiologists’ interpretations and recommendations are carried out downstream in variable ways by other members of the clinical team.
Screening mammography, however, is a less encumbered imaging episode of care. Unlike diagnostic mammography, where in many circumstances the clinical presentation (e.g., palpable mass) dictates services rendered downstream from the mammogram, screening mammography follow-up is almost always the result of that imaging study only and often is directed by the radiologist. Variability in the delivery of services from the clear beginning of the episode (i.e., at the time of the screening examination) until the discrete endpoint of the episode (i.e., a definitive or presumptive benign or malignant diagnosis) is in large part driven by radiologists. Analysis of that variability, with regard to utilization, costs, and outcomes, would similarly help identify excessive, unjustifiable, or low utility care (as in our inpatient model) to preferentially drive value. More importantly, targeted analysis using national benchmarks would, as with our inpatient episodic model, create rich opportunities to share best-practice care delivery methods with radiologists, facilities, and other stakeholders (Figure 2).
 |
| click image to enlarge |
Figure 2: A screening outpatient mammography imaging episode of care entails all imaging services from the start of the episode (the time of the screening mammogram) until the end of the episode (establishment of a definitive or empiric benign or malignant diagnosis). Variation in use of various imaging and procedural services during that episode can be identified and analyzed using administrative health record big data.
Most services provided during a screening mammogram episode of care can be uniquely identified from 5 percent Medicare Part B LDS and similar big data files, making such an episode uniquely suited for our pilot work. Experience from this effort is projected to be translatable to emerging screening services (e.g., low-dose CT for lung cancer in high-risk patients) or selected instances where repeat testing is warranted but currently variably performed (e.g., abdominal incidentaloma or solitary pulmonary nodule follow-up). In these instances, it is largely the imaging findings themselves—rather than the clinical presentation—that drive downstream care in the episode.
Future Trends
Although big data episodic analytics can provide valuable information to align physician specialist roles with sustainable care delivery models, ultimately, patient care must be driven by the evidence-based clinical criteria underneath each utilization decision and their associated costs. Considering again the case of imaging services, one model for managing inpatient care cost and quality would incentivize (or perhaps require) treating physicians to employ clinical decision support systems with embedded appropriateness criteria at the time of requests for imaging services. Such processes would ideally be coordinated with real-time interactivity with radiologists. For screening mammography, reporting decision support systems (either encouraged or perhaps even mandated) would provide similar functionality. Under such models, the baseline payment for imaging associated with an MS-DRG or for an imaging episode would be grounded in the typical cost for an appropriate range of services indicated by both clinical guidelines and empiric claims data. This would help safeguard patients from the potentially damaging incentives of providers inappropriately withholding services to maximize their profits from shared savings, and provide another level of patient protection beyond that offered by outcomes metrics alone.
Of course, because of the idiosyncratic nature of individual patient encounters, many patients will not fit into the one-size-fits-all nature of either ordering or reporting decision support. There must be a mechanism, and appropriate payment, for physicians to effortlessly request specialty consultations or render unique patient-focused services in situations not comporting to established decision support logic. This returns both models to the use of big data. By comparing the annual aggregate use of services to the recommendations provided by decision support systems or nationally accepted guidelines, providers who consistently utilize services in excess of established clinical criteria can be easily identified. Their care patterns could be examined to determine whether their underlying patient populations support a higher level of seemingly lower utility imaging or whether providers are simply delivering an unjustifiable high level of care. Shared savings and risk models could be employed to align provider behavior—of both ordering physician and providing radiologist—with overall health care delivery system goals.
Although these models of specialty care are presented from the vantage point of imaging services, they could be easily adapted to other specialties as well. In fact, since most visible recent efforts have focused on patient length of stay and readmission rates, considerable opportunities exist to address the unique roles of traditional hospital-based physicians—radiologists, pathologists, and anesthesiologists—who typically do not serve as treating physicians but nonetheless provide considerable care that affects patient outcomes. Our screening model additionally offers a platform for studying outpatient episodes of care that remain challenging to define and evaluate for most primary care and specialty providers.
Specialist-focused inpatient MS-DRG and claims-based screening imaging episode benchmarking are but two models for redesigning specialist care payments. As new tools are developed to leverage the potential of big data analytics, additional models, particularly those that better incorporate comprehensive patient clinical data and real-time analysis, are likely to emerge as a result of such pilot model innovation.
